Part 1
All participants received both eculizumab and EMPAVELI
For questions about financial assistance, call 1-866-MY-APL-ASSIST
Jonathan is an adult with PNH who’s taken EMPAVELI
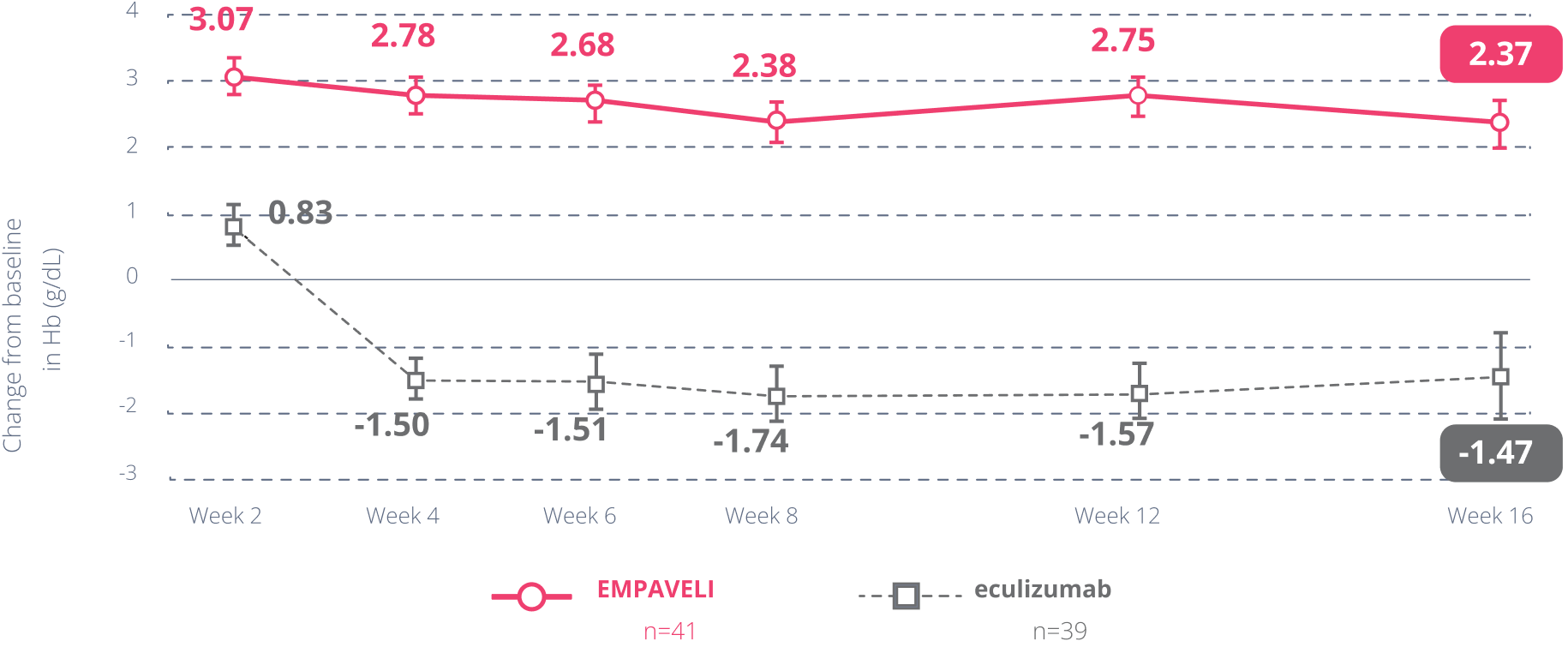
PEGASUS was a study of 80 adults with PNH who had previously taken a C5 inhibitorC5 inhibitorA treatment that targets the C5 protein in the complement system (part of the immune system). C5 is a protein located in the blood that plays an important role contributing to inflammation and intravascular hemolysis caused by the complement system. treatment (eculizumab). The study explored whether EMPAVELI was better at improving hemoglobin than a C5 inhibitor (eculizumab) at Week 16. After that time, patients taking eculizumab were switched to EMPAVELI, and all patients were observed for an additional 32 weeks.
The study consisted of 3 parts:
The primary goal was:
Some of the secondary goals were:
†Noninferiority tests were used for these secondary goals. These statistical tests determined if EMPAVELI was no worse than a C5 inhibitor (eculizumab).
Higher hemoglobin is a key goal in managing PNH, as it helps your red blood cells carry more oxygen throughout your body.

“After being on EMPAVELI for a few months, my hemoglobin went up to 12, which was a great improvement for me. That number has remained steady since I’ve been on the treatment.”
At Week 16 in PEGASUS, EMPAVELI was no worse than a C5i (eculizumab) in helping people with PNH become transfusion free.
Most people on EMPAVELI did not need transfusions after 16 weeks, while most on a C5 inhibitor (eculizumab) did.

Jonathan is an adult with PNH who’s taken EMPAVELI
“I have always used my personal time off for infusions or transfusions. I have never thought about what I can really do with
that time until now.
”
Individual experiences may vary.
The study looked at something called absolute reticulocyte count (ARC). Reticulocytes are new, immature red blood cells. A high ARC can be a sign that your body is working hard to replace red blood cells being destroyed by PNH. A lower ARC can be a sign that this destruction is better controlled.
At Week 16, EMPAVELI was no worse than a C5i (eculizumab) in helping people with PNH reduce their ARC. EMPAVELI was effective at lowering ARC.
The study also observed changes in lactate dehydrogenase (LDH), another marker of red blood cell destruction. It is important to know that these findings are observational, and we cannot draw firm conclusions from them. At Week 16, it could not be determined if EMPAVELI was better or worse than a C5i (eculizumab) at reducing LDH.
Although it was not formally tested, people in the study were asked to report their changes in fatigue levels at Week 16.
This information is for observation only and no conclusions can be made on the effect of EMPAVELI on fatigue. No comparisons can be made between those taking EMPAVELI and those taking eculizumab.
Patients with PNH suffer from persistent anemia, which can cause ongoing symptoms of fatigue because there are not enough red blood cells to carry oxygen throughout the body. Fatigue is a common symptom in patients with PNH.
Average FACIT-Fatigue scores from
beginning of study through Week 16
These data include people who did and did not get a transfusion during the study.
Average FACIT-Fatigue scores from beginning of study through Week 16
These data include people who did and did not get a transfusion during the study.
These data include people who did and did not get a transfusion during the study.
These data include people who did and did not get a transfusion during the study.
The scale ranges from 0 to 52. Higher scores mean less fatigue.
Compared to fatigue scores at the beginning of the study:
People taking EMPAVELI demonstrated
an average improvement of 9.2 points
People taking a C5i (eculizumab) demonstrated
an average decrease of -2.7 points
Report of fatigue may be an under- or overestimation since participants were aware of the treatment they were being given.

Bob is an adult with PNH who’s taken EMPAVELI
“I have had more energy and have been able to get back to the things I enjoy doing without feeling as much intense fatigue as I felt before.”
Individual experiences may vary.
“I’ve been on EMPAVELI for a couple of years now, and my labs have been pretty steady, remaining in a good range. I feel much better now than I did before EMPAVELI.”
Cathy is an adult with PNH who’s taken EMPAVELI
PRINCE was a study of 53 adults with PNH that looked at the effectiveness of EMPAVELI in people who had not been previously treated with a complement inhibitor. The study, which lasted 26 weeks, is explained in more detail in the pop ups below.
The primary goals were:
Selected secondary goal was:
In people who had never received a complement inhibitor
Hb stabilization*
*Hb stabilization means avoiding a >1 g/dL decrease in Hb levels throughout the study.
LDH reduction
For people taking EMPAVELI, average LDH levels in the EMPAVELI group had dropped
from baseline (starting values) at Week 2 and remained there through 26 weeks
At Week 26, patients saw average reductions in their LDH levels compared with their levels before treatment began (their baseline [starting values])
†Control arm (excluding complement inhibitors) only includes data on or before escape (switching to EMPAVELI).
LDH reduction
For people taking EMPAVELI, average LDH levels in the EMPAVELI group had dropped from baseline (starting values) at Week 2 and remained there through 26 weeks
At Week 26, patients saw average reductions in their LDH levels compared with their levels before treatment began (their baseline [starting values])
†Control arm (excluding complement inhibitors) only includes data on or before escape (switching to EMPAVELI).
Most people taking EMPAVELI did not need transfusions through 26 weeks
In an integrated analysis of both the PEGASUS and PRINCE trials, an open-label extension study included adults with PNH who enrolled and had previously completed the PEGASUS study (n=64). Long-term data presented are from an analysis of data in the subset of people who received 1080 mg of EMPAVELI by subcutaneous infusion twice weekly, or every 3 days, for up to 3 years.
The goal of this analysis was to evaluate the long-term effectiveness and safety of EMPAVELI in adults with PNH.
LIMITATIONS
*A run-in phase describes the time between patient recruitment and randomization in a clinical trial, when all of the patients receive the same treatment, which may be a medication, a placebo, or no treatment at all to screen out certain patients.
Average Hb levels over 3 years
Patients who had a transfusion were not included in the Hb analysis for 60 days after the transfusion.
†12 g/dL to 16 g/dL for females, 13.6 g/dL to 18 g/dL for males.
Average LDH levels over 3 years
In an integrated analysis of both the PEGASUS and PRINCE trials, an open-label extension study included adults with PNH who enrolled and had previously completed the PRINCE study (n=50). Long-term data presented are from an analysis of data in the subset of people who received 1080 mg of EMPAVELI by subcutaneous infusion twice weekly, or every 3 days, for up to 2.5 years. This long-term study included patients from another subset, which is not shown below.
The goal of this analysis was to evaluate the long-term effectiveness and safety of EMPAVELI in treating adults with PNH.
LIMITATIONS
Average Hb levels over 2.5 years
Patients who had a transfusion were not included in the Hb analysis for 60 days after the transfusion.
‡12 g/dL to 16 g/dL for females, 13.6 g/dL to 18 g/dL for males.
Average LDH levels over 2.5 years
FACIT=Functional Assessment of Chronic Illness Therapy; Hb=hemoglobin; PNH=paroxysmal nocturnal hemoglobinuria; SE=standard error.
Hb=hemoglobin; LDH=lactate dehydrogenase; PNH=paroxysmal nocturnal hemoglobinuria; SE=standard error.
Hb=hemoglobin; LDH=lactate dehydrogenase; PNH=paroxysmal nocturnal hemoglobinuria.
EMPAVELI is a medicine that affects your immune system and may lower the ability of your immune system to fight infections.
EMPAVELI increases your chance of getting serious infections caused by encapsulated bacteria such as Streptococcus pneumoniae, Neisseria meningitidis, and Haemophilus influenzae type B. These serious infections may quickly become life-threatening or cause death if not recognized and treated early.
Your healthcare provider will give you a Patient Safety Card about the risk of serious infections. Carry it with you at all times during treatment and for 2 months after your last EMPAVELI dose. Your risk of serious infections may continue for several weeks after your last dose of EMPAVELI. It is important to show this card to any healthcare provider who treats you. This will help them diagnose and treat you quickly.
EMPAVELI is only available through a program called the EMPAVELI Risk Evaluation and Mitigation Strategy (REMS). Before you can take EMPAVELI, your healthcare provider must enroll in the EMPAVELI REMS program, counsel you about the risk of serious infections caused by certain bacteria, give you information about the symptoms of serious infections, make sure that you are vaccinated against serious infections caused by encapsulated bacteria and that you receive antibiotics if you need to start EMPAVELI right away and you are not up to date on your vaccines, and give you a Patient Safety Card about your risk of serious infections.
Do not take EMPAVELI if you:
Before you take EMPAVELI, tell your healthcare provider about all of your medical conditions, including if you:
Tell your healthcare provider about all the vaccines you receive and medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements which could affect your treatment.
If you stop taking EMPAVELI, your healthcare provider will need to monitor you closely for at least 8 weeks after stopping EMPAVELI. Stopping treatment with EMPAVELI may cause a breakdown of red blood cells due to PNH.
Symptoms or problems that can happen due to red blood cell breakdown include:
EMPAVELI can cause serious side effects including allergic reactions. Allergic reactions can happen during your EMPAVELI infusion. Stop your EMPAVELI infusion and tell your healthcare provider or get emergency medical care right away if you get any of these symptoms during your EMPAVELI infusion:
The most common side effects in people with PNH treated with EMPAVELI include injection-site reactions; infections; diarrhea; pain in the stomach (abdomen); respiratory tract infection; pain in the arms, hands, legs, or feet; low potassium in blood; tiredness; viral infection; cough; joint pain; dizziness; headache; and rash.
These are not all of the possible side effects of EMPAVELI. Tell your healthcare provider about any side effect that bothers you or that does not go away.
Call your healthcare provider for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
EMPAVELI is a prescription medicine used to treat adults with a disease called paroxysmal nocturnal hemoglobinuria (PNH).
Please see full Prescribing Information, including Boxed WARNING regarding risk of serious infections, and Medication Guide for additional information.
By submitting this form, I acknowledge that I have reviewed, understood, and agree to the below guidelines, that I am at least 18 years of age and am legally competent to enter into this agreement, that I own all rights to the content submitted, and that I have received permission to submit the content from any other individual appearing in my submission for use by Apellis Pharmaceuticals, Inc. (“Apellis”), as set forth below.
Apellis can take, collect and use any content I have submitted to this webpage, including my photographs, film or recordings taken of my image and voice, my quotation or testimonial, as well as any personal health information contained in such photographs, film or recordings or provided on this submission form (collectively, “My Content and Information”). Apellis reserves the right to not post or use My Content and Information.
Apellis and its subsidiaries, affiliates, licensees, successors, assignees and those acting with its authority, have the right to use, re-use, broadcast, display and publish My Content and Information on social media, websites, displays, and emails. I waive all rights that I may have to claims for payment or royalties in connection with the posting or other usage of My Content and Information on these platforms. Apellis will contact me by e-mail or phone if it would like to feature My Content and Information elsewhere.
Any content that I submit to Apellis may be edited or excerpted in Apellis’ sole discretion to align with promotional requirements and the intended use of this site. I waive all rights in My Content and Information, including any right to inspect or approve My Content and Information prior to use or dissemination by Apellis. If significant changes are required, Apellis may contact me via e-mail or phone. Apellis will not use my e-mail address or phone number for any other purpose, unless I have separately opted into receiving communications from Apellis.
Adverse Events (“AEs”): Apellis will address any adverse events or side effects mentioned within submissions according to FDA regulations. You may report side effects to FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Sign up to join the EMPAVELI PNH community:
EMPAVELI is a medicine that affects your immune system and may lower the ability of your immune system to fight infections.
EMPAVELI increases your chance of getting serious infections caused by encapsulated bacteria such as Streptococcus pneumoniae, Neisseria meningitidis, and Haemophilus influenzae type B. These serious infections may quickly become life-threatening or cause death if not recognized and treated early.
Your healthcare provider will give you a Patient Safety Card about the risk of serious infections. Carry it with you at all times during treatment and for 2 months after your last EMPAVELI dose. Your risk of serious infections may continue for several weeks after your last dose of EMPAVELI. It is important to show this card to any healthcare provider who treats you. This will help them diagnose and treat you quickly.
EMPAVELI is only available through a program called the EMPAVELI Risk Evaluation and Mitigation Strategy (REMS). Before you can take EMPAVELI, your healthcare provider must enroll in the EMPAVELI REMS program, counsel you about the risk of serious infections caused by certain bacteria, give you information about the symptoms of serious infections, make sure that you are vaccinated against serious infections caused by encapsulated bacteria and that you receive antibiotics if you need to start EMPAVELI right away and you are not up to date on your vaccines, and give you a Patient Safety Card about your risk of serious infections.
Do not take EMPAVELI if you:
Before you take EMPAVELI, tell your healthcare provider about all of your medical conditions, including if you:
Tell your healthcare provider about all the vaccines you receive and medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements which could affect your treatment.
If you stop taking EMPAVELI, your healthcare provider will need to monitor you closely for at least 8 weeks after stopping EMPAVELI. Stopping treatment with EMPAVELI may cause a breakdown of red blood cells due to PNH.
Symptoms or problems that can happen due to red blood cell breakdown include:
EMPAVELI can cause serious side effects including allergic reactions. Allergic reactions can happen during your EMPAVELI infusion. Stop your EMPAVELI infusion and tell your healthcare provider or get emergency medical care right away if you get any of these symptoms during your EMPAVELI infusion:
The most common side effects in people with PNH treated with EMPAVELI include injection-site reactions; infections; diarrhea; pain in the stomach (abdomen); respiratory tract infection; pain in the arms, hands, legs, or feet; low potassium in blood; tiredness; viral infection; cough; joint pain; dizziness; headache; and rash.
These are not all of the possible side effects of EMPAVELI. Tell your healthcare provider about any side effect that bothers you or that does not go away.
Call your healthcare provider for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
EMPAVELI is a prescription medicine used to treat adults with a disease called paroxysmal nocturnal hemoglobinuria (PNH).
Please see full Prescribing Information, including Boxed WARNING regarding risk of serious infections, and Medication Guide for additional information.